Diabetes is a complex metabolic disease that affects the entire vascular system of the body, including the eyes, giving rise to specific changes generically called diabetic retinopathy.
Symptoms of diabetes are frequent urination, abnormal thirst, abnormal hunger, anemia, fatigue, weight loss, etc.. Diagnosis is made by your doctor, based on clinical and laboratory investigations.
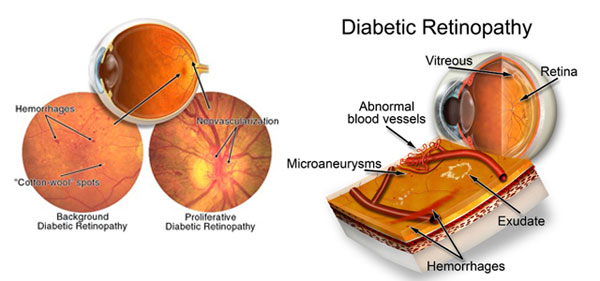
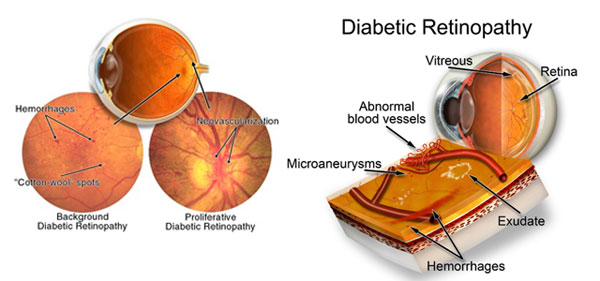
Diabetic retinopathy is a disease of the blood vessels that nourish the retina: they are weak, they break and “escape” fluid and blood in the retina (retinal hemorrhages), in addition, these blood vessels do not manage to bring nutrients and oxygen needed by retina (hypoxia), doing even more damage. Evolution is progressive, in years, and without proper treatment, this inevitably leads to blindness.
The causes are not fully known, but once installed, its evolution cannot be stopped, only slowed or maintained, and therefore, its early detection is essential, regardless of the glucose level.
In early stages, diabetic retinopathy has no symptoms (loss of vision, pain or other signs), so all patients diagnosed with diabetes should carry out an eye test periodically (1-2 times per year), for early detection of retinal changes. It is very important to begin an effective treatment as soon as possible, when the disease is still in its infancy state.
Diagnostic methods:
– Ophthalmic clinical examination with visual acuity measurements.
– Examination of the bottom of the eye.
– Fluorescein angiography is a method used after diabetic retinopathy has been diagnosed to determine how severe the damage to the retina is, it consists of a successive series of photographs of the eye, which give a clearer picture of the lesions in the retina.
– Color stereoscopic photos of the eye – to better showcase the lesions, and to watch their evolution in time.
– Retinal Tomography – OCT – can diagnose some complications in the retina.
– Posterior pole ultrasound exam) – for detecting proliferation of retinal detachment.
Treatment of diabetic retinopathy:
Treatment consists in monitoring and treatment of diabetes itself, as well as monitoring and specific treatment of diabetic retinopathy, by an ophthalmologist specialised in retinal diseases.
Once the treatment is started, diabetic retinopathy will continue to exist even if the patient has a normal blood-sugar level due to general anti-diabetic treatment.
Treatment of diabetic retinopathy depends on the location and severity of the disease. When the affected area is the peripheral retina and damages are found early, treatment and careful monitoring of the disease are continued. When the affected area is the macula (the center of the retina), laser treatment is necessary, in regular sessions.
In proliferative diabetic retinopathy (already advanced), laser treatment is used to stop the emergence and development of new blood vessels (laser points apply throughout the retina).
In advanced cases are required complex operations on the retina – vitrectomy using laser applications, followed by injection with expandable gas or silicone oil – as appropriate.